Pharmacy Information for Members
Medication Formularies:
“To search the formulary, press Ctrl F and type in the drug name you are looking for.”
Mail-Order Medications:
Please contact Postal Prescription Services (PPS) at 800-552-6694 to establish a new member profile. Advanced Health members are enrolled under “Doctors of the Oregon Coast” plan. New member profile and prescription transfer requests may be made by phone. PPS Customer New Prescription Request PPS Mail-Order Quick Reference Guide
If you would like a printed copy of our Drug Formulary, it is available to you at no charge and will be provided to you within 5 business days of your request. Please call customer service at 541-269-7400, 1-800-264-0014 or TTY 711 or 800-735-1232.
- A formulary is a list of medicines that are covered for Advanced Health members.
- Some medicine requires a prior authorization before Advanced Health will pay for the prescription.
- If you are prescribed a medication that is not on the Advanced Health formulary, please contact your provider and ask them to change you to a medication that is on the formulary.
- If there is no medicine on the formulary that can be used to treat your condition, please request that your provider submit a prior authorization to Advanced Health.
- Having your provider send us a prior authorization does not guarantee that your medicine will be paid for by Advanced Health.
- Generic medicine must be used to fill your prescription when available. Generic medicines work the same as brand name medicines.
- There is no copay for prescriptions that are covered by Advanced Health.
- Some medicines are paid for directly by the State of Oregon, not by Advanced Health. These are medicines that are used to treat mental health conditions, such as antidepressants.
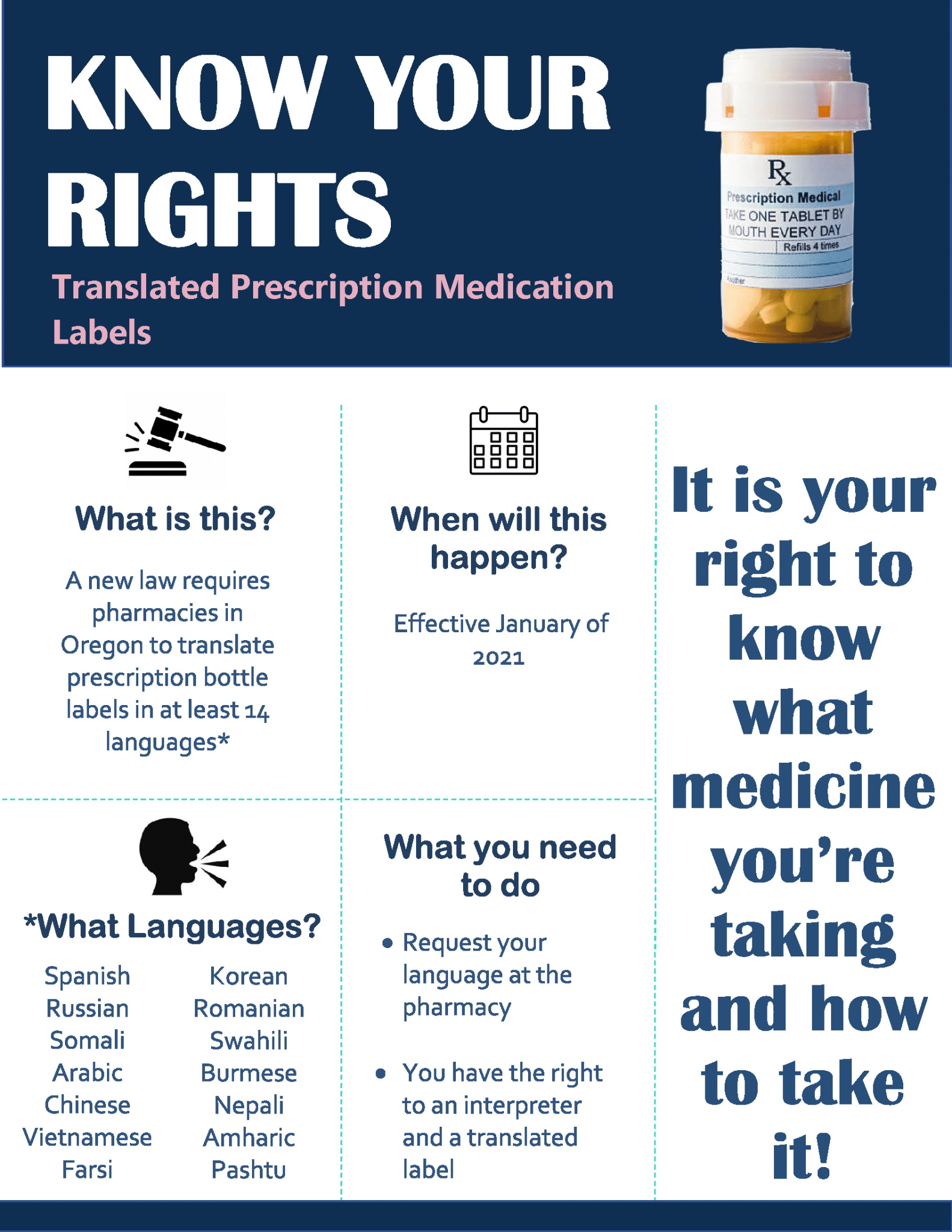
- You may fill your prescription at any local pharmacy, except Walgreens who does not contract with Advanced Health.
- If you are on vacation in Oregon, you may fill your prescription at most major chain pharmacies. Please take your prescription bottle to the pharmacy where you are visiting and they will transfer the prescription. Please note special regulations apply to controlled substances. All Federal and State requirements must be followed. If you are planning a vacation outside of Oregon and will need a refill of your medicine before you return, please call your pharmacy and request a refill. Your pharmacy may call the Advanced Health Pharmacy department and request a vacation override for your trip. Please take your Advanced Health identification number with you to the pharmacy every time you need a prescription filled.
- Please contact Advanced Health Member Services at (541) 269-7400 if you have any questions or need assistance.
Medication Disposal:
**It is important that we discard prescriptions and over-the-counter medications correctly. Having unused or expired medicine around your house can also lead to accidental poisoning and can be harmful to children or teens. So please take a moment to go through your medicine cabinet and get rid of any medication that you do not take any more or that is expired. Take the unused or expired medications to a local drug disposal site (see the Drug Take Back Sites list below). There is likely one near where you live. If there are no drop boxes or other safe disposal sites near you, the FDA recommends mixing unused medications in with used coffee grounds and throwing it out or flushing it down the toilet. (Please see the EPA step by step procedure below)
- Drug Take Back Sites
- Stay Safe Oregon Website
- EPA-How to Dispose of Medicines Properly
- BAH – HOW TO DISPOSE OF SHARPS CONTAINERS
**For a Pain Management guidance and tool for patients and their families, click the link below. The Oregon Pain Guidance (OPG) is a group of healthcare providers from Jackson and Josephine Counties in Southern Oregon, who are working together on standardizing community guidelines and best practices for treating patients with chronic pain. An improved quality of life for people with chronic pain can be achieved when patients and their families work closely with their healthcare providers. This website provides educational information, new, community resources and upcoming events for both the public and healthcare providers. http://www.oregonpainguidance.com/patients-families/